From Advances in Neonatal Care
Guide to a Systematic Physical Assessment in the Infant With Suspected Infection and/or Sepsis
Published: 09/02/2004
Abstract and Introduction
Abstract
This article provides the resources for the bedside caregiver to conduct a focused physical assessment of the infant with suspected sepsis. The importance of obtaining a complete history to identify associated obstetric and neonatal risk factors is emphasized. Further evaluation of the infant's clinical presentation for signs and symptoms suggestive of a systemic inflammatory response to infection is discussed, along with a step-by-step guide to a systematic physical assessment. Strategies to evaluate physical findings in context with the available diagnostic data to develop a differential diagnosis are provided. The international consensus definitions for the sepsis continuum are presented and are compared and contrasted to the definitions more commonly used in the neonatal population. The article provides tables that can serve as checklists to structure a thorough obstetric and neonatal history and to further evaluate the infant's systemic inflammatory response to infection.
Introduction
The diagnosis of sepsis is challenging due to the nonspecific nature of clinical presentation, the variety of other neonatal disorders within the differential diagnostic workup, and the lack of sensitivity and specificity of available diagnostic procedures. Despite advances in the understanding of the pathophysiology of sepsis, the treatment remains primarily supportive in nature.
Mortality from sepsis depends on case definitions, the presence of shock, as well as the presence of underlying diseases. In children, mortality most often occurs in the first 48 hours of infection.[1] In a recent epidemiologic evaluation of severe sepsis in children in the United States, the estimated annual incidence of severe sepsis in newborns was 0.3 per 100 live births.[2] Of the newborns with severe sepsis in the 5-state cohort, 81.1% were low birth weight (LBW; <2500 grams) and 63.6% were very low birth weight (VLBW; <1500 grams). The estimated case mortality rate was 10.3%.
The National Institute of Child Health and Human Development (NICHD) Neonatal Research Network reported the incidence of late-onset sepsis, defined as a positive result on one or more blood cultures obtained after 72 hours of life.[3] Of the 6215 infants who survived beyond 3 days, 1313 (21%) had one or more episodes of blood-culture proven sepsis, resulting in significantly longer hospital stays and higher mortality than infants without late-onset sepsis.
Sepsis occurs across a continuum beginning with infection, systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic shock, and may culminate with multiple organ dysfunction syndrome. International consensus definitions have been adapted for pediatric use; these definitions have not been widely accepted in the neonatal literature. Table 1 compares the international consensus definitions of sepsis to those used by the Vermont Oxford Network and NICHD Neonatal Research Network.[4-8] The use of consensus definitions facilitates consistency in terminology and diagnostic criteria so that results of research studies related to sepsis can be compared.
Table 1.
| Sepsis Terminology | ACCP/SCCM Consensus[4,5] | ACCP/SCCM Sepsis Terminology Adapted for Children[6] | Vermont Oxford Network Release 8.07 | National Institute of Child Health and Human DevelopmentNeonatal Research Network[8] |
|---|---|---|---|---|
| Infection | Microbial phenomenon characterized by an inflammatory response to the presence of microorganisms or the invasion of normally sterile host tissue by those organisms. | Same. | Not defined. |
Intra-uterine infection:
Congenitally infected with any TORCH virus, infants born to mothers with untreated syphilis, and infants born to HIV positive mothers |
|
Late-onset culture negative infection:
Negative blood culture obtained (>72 hours) and treated with antibiotics for ≥5 days. |
||||
|
Infection of meninges/brain:
Positive culture of CSF or pathogens in brain tissue in the presence of compatible signs of meningitis or encephalitis |
||||
|
Suspected sepsis/infection (as a cause of death):
Clinical presentation of septicemia or localized infection without positive cultures during life or on autopsy |
||||
|
Proven sepsis/infection (as a cause of death):
Septicemia or localized infection with positive blood or organ cultures (for example, septicemia, meningitis, pulmonary abscess, etc.) |
||||
| Bacteremia | The presence of viable bacteria in the blood. | Same. | Not defined. | Same definition as early onset septicemia. |
| Systemic Inflammatory Response Syndrome (SIRS) | The systemic inflammatory response to a variety of severe clinical insults. The response is manifested by 2 or more of the following conditions: temperature >38°C or <36°C; heart rate >90 beats per minute; respiratory rate >20 breaths per minute or pCO2 <32 mm Hg; and white blood cell count >12,000/mm3, <4000/mm3, or >10% immature (band) forms. | The systemic response to a variety of clinical insults (infection, trauma, and burns). The response is manifested by 2 or more of the following: Temperature >38°C or <36°C; heart rate >2 SD above age normal; respiratory rate >2 SD above age normal; leukocyte count >12,000 cells/mm3, <4,000 cells/mm3, or >10% band forms. | Not defined. | Not defined. |
| Sepsis | The systemic response to infection manifested by 2 or more of the following conditions as a result of infection: temperature >38°C or <36°C; heart rate >90 beats per minute; respiratory rate >20 breaths per minute or pCO2 <32 mm Hg; and white blood cell count >12,000/mm3, <4000/mm3, or >10% immature (band) forms. | (SIRS plus infection). The systemic response to infection manifested by 2 or more of the following: Temperature >38°C or <36°C; heart rate >2 SD above age normal; respiratory rate >2 SD above age normal; leukocyte count >12,000 cells/mm3, <4000 cells/mm3, or >10% band forms. |
Bacterial Sepsis Early:
Bacterial pathogen* was recovered from a blood culture and/or CSF culture obtained on day 1, 2, or 3 of life. |
Early onset septicemia/bacteremia:
Positive blood culture drawn within the first 72 hours. |
|
Late onset septicemia/bacteremia:
Positive culture of blood obtained in the presence of clinical signs of septicemia, occurring after 72 hours. |
||||
|
Suspected sepsis/infection (as a cause of death):
Clinical presentation of septicemia or localized infection without positive cultures during life or on autopsy. |
||||
|
Proven sepsis/infection (as a cause of death):
Septicemia or localized infection with positive blood or organ cultures (for example septicemia, meningitis, pulmonary abscess, etc.). |
||||
| Severe sepsis | Sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Hypoperfusion and perfusion abnormalities may include, but are not limited to, lactic acidosis, oliguria, or an acute alteration in mental status. | Same. | Not defined. | Not defined. |
| Septic shock | Sepsis-induced hypotension despite fluid resuscitation along with the presence of perfusion abnormalities that may include, but are not limited to, lactic acidosis, oliguria, or an acute alteration in mental status. Patients who are receiving inotropic or vasopressor agents may not be hypotensive at the time that perfusion abnormalities are measured. | Same. | Not defined. | Not defined. |
| Sepsis-induced hypotension | A systolic blood pressure <90 mm Hg or a reduction of >40 mm Hg from baseline in the absence of other causes for hypotension. | A systolic blood pressure reading more than 2 SD below the mean for the age. | Not defined. | Not defined. |
| Multiple Organ Dysfunction Syndrome (MODS) | Presence of altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention. | Same. | Not defined. | Not defined. |
Abbreviations: ACCP, American College of Chest Physicians; CSF, cerebrospinal fluid; CONS, coagulase negative straphylococcus; HIV, human immunodeficiency virus; IV, intravenous; SCCM, Society of Critical Care Medicine; TORCH, toxoplasmosis, rubella, cytomegalovirus and herpes.
*Specified list of pathogens.
Table 1. Comparison of ACCP/SCCM Consensus Definitions for Adults and Adaptation for Children With Definitions Utilized by Neonatal Research Networks[4-8]
A suggestive diagnosis of sepsis is made based on clinical symptomatology and elimination of other possible causes of the patient's condition. A definitive diagnosis for sepsis is made only with a documented Systemic Inflammatory Response Syndrome (SIRS) and a definitive microbial cause of infection.[4,5]
The definitions for sepsis continue to evolve. In 2001, an International Sepsis Definitions Conference concluded that the SIRS criteria were overly sensitive and nonspecific and recommended an expanded list of signs and symptoms of sepsis that may better reflect clinical responses to infection. Table 2 lists the possible signs of systemic inflammation, which incorporates physical and laboratory findings that prompt an experienced clinician to determine if an infected patient has sepsis.[4] In this article focused on the physical assessment, the international consensus definition of sepsis, that is, the presence of SIRS with infection, is used.
Table 2.
|
General parameters Infection* documented or suspected and some of the following:
Inflammatory parameters
Hemodynamic parameters
Organ dysfunction parameters
Tissue perfusion parameters
|
Reproduced with permission.[4]
*Defined as a pathological process induced by a microorganism.
Values above 70% are normal in children (normally 75% to 80%) and should therefore not be used as a sign of sepsis in newborns or children.
Values of 3.5 to 5.5 are normal in children and should therefore not be used as a sign of sepsis in newborns or children.
Table 2. Possible Signs of Systemic Inflammation in Response to Infection[4]
Obtain a Focused History
Infants have a predisposition to infection. The pathogenesis of this predilection includes a complex interaction between obstetric and newborn factors; therefore, both the mother's and the infant's history are critical to a comprehensive risk assessment.
Obstetrical History
Review the obstetrical history including maternal health before pregnancy, prenatal care and events, as well as antepartum and intrapartum events. Any risk factor associated with preterm labor, LBW, or premature birth is a risk factor for neonatal sepsis. In some cases, an acute or subclinical maternal infection may have been the basis for preterm labor, increasing the risk for early onset infection or sepsis (onset <3 to 5 days of age).
Many pre-existing maternal health conditions are associated with premature birth and/or LBW. Maternal health behavior during pregnancy also impacts the neonate's risk for sepsis. Poor nutrition, smoking, and alcohol and drug use during pregnancy are linked to both LBW and premature birth. Obstetrical complications tend to be risk factors for early-onset sepsis; drug use and environmental exposures increase the risk of anatomical defects, which are neonatal risk factors for late-onset sepsis.[9,10] The rate of late-onset sepsis is also inversely related to birth weight and gestational age.[3] Table 3 outlines obstetric risk factors for infection and/or sepsis and can be used as a checklist in the history taking process.[9-13]
Table 3.
|
Pre-existing Maternal Health Conditions
Maternal Health Behavior During Pregnancy
Obstetrical Complications
Intrapartum Complications
|
Table 3. Obstetrical Risk Factors for Neonatal Infection/Sepsis[9-13]
Neonatal History
After reviewing the maternal history, focus on the events surrounding the labor, the delivery, the infant's need for resuscitation, measures used in the early stabilization, and the infant's initial clinical course. Being cared for in a neonatal intensive care unit (NICU) is a risk factor for late-onset sepsis due to invasive medical procedures and environmental issues.[9-10] Table 4 outlines additional neonatal risk factors for infection and/or sepsis.[3,9-13]
Table 4.
|
Immaturity of Immune System [11]
Anatomic Defects (late onset >3-5 days) [9,10]
NICU Care/Environmental Issues (late onset >3-5 days) [9,10]
Poor Nutrition [3]
Complications of Prematurity [3]
|
Table 4. Neonatal Risk Factors for Infection/Sepsis[3,9-11]
In newborns, infection frequently presents with minimal or nonspecific symptoms. Early warning signs are subtle and can be confused with apnea of prematurity, environmental temperature variation, or acute exacerbation of chronic lung disease. In contrast, some infants progress rapidly along the sepsis continuum, presenting with alarmingly fulminant progressive symptoms.[14]
The revised definition of SIRS, outlined in Table 2 , includes laboratory findings and clinical signs of early organ dysfunction associated with sepsis. Table 4 lists neonatal specific risk factors. Use Table 2 and Table 4 as checklists in your review of the infant's medical records to perform a risk assessment.
Table 2.
|
General parameters Infection* documented or suspected and some of the following:
Inflammatory parameters
Hemodynamic parameters
Organ dysfunction parameters
Tissue perfusion parameters
|
Reproduced with permission.[4]
*Defined as a pathological process induced by a microorganism.
Values above 70% are normal in children (normally 75% to 80%) and should therefore not be used as a sign of sepsis in newborns or children.
Values of 3.5 to 5.5 are normal in children and should therefore not be used as a sign of sepsis in newborns or children.
Table 2. Possible Signs of Systemic Inflammation in Response to Infection[4]
Table 4.
|
Immaturity of Immune System [11]
Anatomic Defects (late onset >3-5 days) [9,10]
NICU Care/Environmental Issues (late onset >3-5 days) [9,10]
Poor Nutrition [3]
Complications of Prematurity [3]
|
Table 4. Neonatal Risk Factors for Infection/Sepsis[3,9-11]
Table 2.
|
General parameters Infection* documented or suspected and some of the following:
Inflammatory parameters
Hemodynamic parameters
Organ dysfunction parameters
Tissue perfusion parameters
|
Reproduced with permission.[4]
*Defined as a pathological process induced by a microorganism.
Values above 70% are normal in children (normally 75% to 80%) and should therefore not be used as a sign of sepsis in newborns or children.
Values of 3.5 to 5.5 are normal in children and should therefore not be used as a sign of sepsis in newborns or children.
Table 2. Possible Signs of Systemic Inflammation in Response to Infection[4]
Table 4.
|
Immaturity of Immune System [11]
Anatomic Defects (late onset >3-5 days) [9,10]
NICU Care/Environmental Issues (late onset >3-5 days) [9,10]
Poor Nutrition [3]
Complications of Prematurity [3]
|
Table 4. Neonatal Risk Factors for Infection/Sepsis[3,9-11]
Physical Assessment
When used alone, the physical assessment lacks sensitivity and specificity in identifying sepsis. A single assessment provides only a snapshot of information that must be viewed in context with the neonatal history and other diagnostic data. Serial physical assessments can aid in the identification of infection and sepsis. This discussion of physical assessment is intended to assist the bedside provider in early recognition of sepsis, irrespective of causative pathogens. It is not intended to be a comprehensive discussion of the physical assessment of an infant.
The physical assessment of an infant includes observation, auscultation, and palpation proceeding in a systematic head-to-toe fashion. To provide quality data, the assessment is organized to minimize stress for the infant. Observation precedes auscultation and palpation so as not to disturb the infant. Palpation is the last aspect of the physical assessment because it frequently results in agitation.
Begin the assessment by evaluating vital sign trends. Temperature instability is a common finding in infection and can present as fever or, more commonly in the premature infant, hypothermia. Temperature fluctuations may be masked when the infant's thermal management is in the servo-control mode of a radiant warmer or incubator.
In servo-control mode, the desired infant skin temperature is used as a set point. The incubator or warmer then gradually increases or decreases heat output as needed to maintain the infant's skin temperature at the desired set point. To evaluate temperature instability when the infant's incubator or warmer is in servo-control mode, look for fluctuations in the environmental temperatures that were required to keep the infant's skin temperature at the set point.
Also, evaluate vital sign trends for changes in heart rate, specifically resting tachycardia. This may signal intravascular depletion, and commonly precedes a drop in blood pressure. Review blood pressure trends. Umbilical artery catheter pressures are typically the most reliable measurement.
Observation
Observation provides significant information on the general condition of the infant. Observe the infant at rest before any manipulation noting the behavior and sleep state of the infant. Evaluate for changes in activity and behavior state throughout the examination. Normally the state of an infant fluctuates between sleep states (deep sleep, light sleep) and awake states (drowsy, quiet alert, active alert).[15]
A change in mental status is part of a clinical triad that can help caregivers identify septic shock before hypotension occurs.[16] This triad includes:
|
In infants, a change in mental status is observed through a change in sleep states and behavior. Crying is a normal response to manipulation, undressing, and handling during a physical examination. Either the inability to be aroused, manifested by a lack of crying or evasive movement during the examination, or inconsolable crying may be indicative of sepsis.[16,17]
Carefully observe the infant for signs and symptoms of meningitis. Approximately one third of neonatal cases of sepsis are associated with meningitis.[18] Irritability, lethargy, a high-pitched cry, nuchal rigidity, and seizure activity are findings that, if present, can be associated with meningitis. Conversely, absence of these signs does not rule out meningitis.
Assess the infant's position of comfort and overall tone. The premature infant, whose muscle tone is less mature, has a more extended position of extremities as compared to the increasing flexion of the upper and lower extremities that is noted at term. Flexion of the lower extremities precedes flexion in the upper extremities. Although infrequently seen, an exaggerated arched position of the head and neck, termed opisthotonos, can be indicative of meningitis (Fig 1).

Figure 1. Note the opisthotonos exhibited by this infant. Ospithotonic positioning may be a sign of meningitis, or alternatively, may be seen in an infant who is attempting to compensate for airway edema or stridor. Reprinted with permission from Clark D. Atlas of Neonatology. Philadelphia, Pa: WB Saunders; 2000:134.
Observe the infant's movements at rest. Movements of the upper and lower extremities should be spontaneous and symmetrical. Activity, reactivity, and tone should be appropriate for the infant's adjusted gestational age; each element increases with increasing gestational age and maturity. Seizure activity, lethargy, and poor tone may be associated with sepsis (Fig 2). Assess the facial activity of the infant. Observe for eye movement, nasal flaring, and presence or absence of the suck reflex.

Figure 2. Hypotonia. Note the generalized symmetrical hypotonia in an infant with suspected sepsis. Photograph courtesy of Dr. David Clark, Albany Medical Center, Albany, New York.
Observe the general appearance of the infant's skin. Hematologic problems associated with sepsis may present clinically as petechiae (Fig 3A) or purpura (Fig 3B). Hemostatic activation, which manifests clinically as coagulopathy of sepsis, is nearly universal (98%) in patients with severe sepsis.[19] Petechiae confined to the presenting part may be a normal finding after a vaginal delivery or a prolonged labor. Generalized petechiae may indicate thrombocytopenia. Blood oozing from venepuncture sites or excessive bruising may indicate disseminated intravascular coagulation.
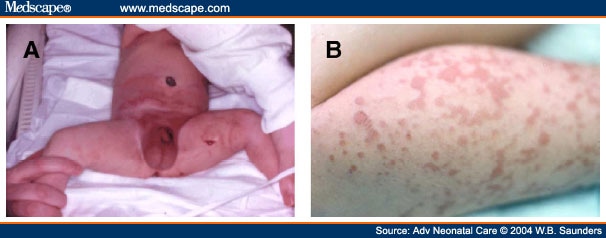
Figure 3. (A) Petechiae. Infant with an infected plastibell circumcision; the responsible organism was Group B streptococcus. Note the scattered petechiae surrounding the penis and extending upward to the periumbilical area. Photo courtesy of Dr. William Edwards, the Children's Hospital at Dartmouth. (B) Purpura. Note the area of small hemorrhages on the right leg of this infant compared to the petechiae (minute, pinpoint-sized hemorrhages) in Figure 3A. Purpura is often associated with decreased platelet counts.
Septic shock can be recognized before hypotension occurs by noting a change in perfusion, resulting in either peripheral vasodilation (warm shock) or cool extremities (cool shock).[16] In a warm shock state, the appearance of the skin is flushed; a cold shock state is characterized by a mottled or bluish discoloration of the skin (Fig 4).

Figure 4. Note the diffuse mottled, bluish-gray appearance of this infant's skin suggestive of systemic poor perfusion. Photograph courtesy of Dr. David Clark, Albany Medical Center, Albany, New York.
Assess the skin color, in natural light if possible, for color, integrity, and presence of rash or discolorations. Determine the extent of jaundice by applying gentle pressure to the skin over a bony prominence, such as the face or sternum. Observe the underlying skin for a yellow color. Note the line of demarcation (for example, jaundice to the nipple line). Jaundice in the first 24 hours of life is an abnormal finding and may indicate an underlying infectious etiology; it is present in approximately one third of infants with sepsis.[10] Pallor is an abnormal finding and may be associated with shock. A gray or ashen color may be associated with metabolic acidosis related to sepsis.
Moving in a cephalocaudal direction, the chest is the next focus of observation. Observe respiratory rate, rhythm, and overall effort and work of breathing, while the infant is at rest, before any manipulation. Breathing should be relatively effortless, comfortable, and passive. Note the presence of substernal, sternal, intercostals, or supraclavicular retractions. Retractions indicate that the infant is using accessory muscles, likely in an effort to compensate for respiratory pathology.
Infants with sepsis often present with respiratory symptoms. The clinical symptoms of tachypnea, grunting, flaring, retractions, apnea, and cyanosis are common findings associated with a variety of neonatal respiratory disorders; each disorder will need to be ruled out based on history, risk factors, radiologic findings, and clinical progression and course.
Next, observe the infant's abdomen. Gastrointestinal disturbances are common in neonatal sepsis. Although nonspecific in nature, they may be early significant signs. Assessment of the abdomen includes observation for distension, bowel loops, and erythematous areas (Fig 5). Observe the umbilicus for redness, swelling, drainage, and foul odor (Fig 6). Assess the lower abdomen for evidence of bladder distension. Note the presence, absence, and character of stool and urine and observe the voiding stream if possible.

Figure 5. Abdominal distension is a nonspecific sign of infection and sepsis. Note the presence of bowel loops that are visible through the abdominal wall. Reprinted with permission from Clark D. Atlas of Neonatology. Philadelphia, Pa: WB Saunders; 2000:183.

Figure 6. The umbilical stump is necrotic tissue in the process of separating from the abdominal wall. Omphalitis can present as periumbilical erythema, warmth, or drainage; the infection may be localized or may be a source for a systemic infection. Reprinted with permission from Clark D. Atlas of Neonatology. Philadelphia, Pa: WB Saunders; 2000:63.
Auscultation
Auscultation is the next component in the physical assessment of the infant. Auscultation is most effective when the infant is in a quiet state. Warming of the hands and stethoscope and use of a pacifier are techniques that can assist the infant to maintain a quiet state during auscultation.
Begin with auscultation of the heart. Note the rate, rhythm, presence, location character, and transmission of a murmur and the point of maximum impulse. In the absence of congenital heart disease, clinical signs of cardiovascular dysfunction are sensitive signs of sepsis (tachycardia, arrhythmia, poor perfusion). Infants maintain higher vascular tone than adults. Therefore, in infants with sepsis, the shock state occurs long before hypotension.[4] The newborn has limited capacity to increase stroke volume as a result of few contractile elements and poor innervation of the fetal myocardium. The newborn increases cardiac output primarily by increasing the heart rate, resulting in tachycardia. Tachycardia may be absent in hypothermic infants.[4]
Sepsis-induced acidosis and hypoxemia can increase pulmonary artery pressure, prolonging the patency of the ductus arteriosus (PDA).[16] The murmur associated with a PDA is best heard at the upper left sternal border and is described as a machinery-like murmur. The presence of other murmurs may assist in the differential diagnosis and indicate congenital heart disease.
Next, auscultate the breath sounds. Listen for symmetry of breath sounds, comparing the right side to the left side starting from the top of the chest to the diaphragm and listening over the anterior, medial, and posterior lung fields. Bilateral breath sounds with good air entry are the normal finding. Listen for the presence of crackles (simulated by rolling a lock of hair between fingers near the ear), wheezes (musical quality), and rubs (friction-induced sound simulated by moving a finger tip up and down a hand cupped over your ear). Note the location and phase of respiration of these abnormal breath sounds. The presence of crackles at the end of the inspiratory phase or diminished breath sounds may be indicative of pneumonia. An expiratory grunt is also a nonspecific finding that can be associated with sepsis.
Assessment of the abdomen begins with auscultation of bowel sounds. Listen to all 4 quadrants of the abdomen for the presence or absence of bowel sounds. In infants, approximately 10 to 30 bowel sounds per minute are normal. Diminished bowel sounds may be a clinical finding associated with a paralytic ileus that can be seen in infection. The absence of bowel signs may reflect perforation and potential peritonitis as seen in necrotizing enterocolitis (NEC), one of the most serious gastrointestinal disorders, which is often associated with sepsis.
Palpation
Palpation should proceed in a systematic approach from head to toe. Palpation provides the most useful information when the infant is not crying. With crying, the fontanel and abdominal muscles tense and impact the quality of the data obtained. During palpation, note the infant's response to both superficial and then incrementally deeper palpation. Monitor for facial grimace, guarding, withdrawal, and other signs of pain. Alternatively, those infants who are seriously compromised may be lethargic and fail to withdraw or respond at all. Note the infant's physiologic response to handling, carefully assessing for concomitant desaturation, hypotension, increased work of breathing, or apnea. Compromised infants often have a slow recovery to baseline of their vital signs and physiologic parameters.
Palpate the infant's anterior, posterior, and temporal squamosal fontanel. Ideally, palpation should occur in the upright position; alternatively, hold the infant with the head slightly elevated. A bulging, full, or tense fontanel (Fig 7) may be indicative of increased intracranial pressure and/or meningitis. Further palpate the infant's neck for range of motion, stiffness, lymph nodes, and other masses, lesions, or skin defects.

Figure 7. Palpate the fontanel in the upright position, or with the head supported in a semiupright position. A bulging fontanel may be associated with meningitis. Reprinted with permission from Clark D. Atlas of Neonatology. Philadelphia, Pa: WB Saunders; 2000:135.
Next, place the infant in the supine position with legs flexed to palpate the abdomen. Begin in the lower abdomen and palpate in an upward direction. The liver edge can be easily palpated in preterm infants. It can extend to 2 cm below the costal margin in healthy term infants. Palpation and percussion may provide a more reliable determination of liver span than measurement of projection below the costal margin.
Hepatomegaly may be indicative of an intrauterine infection. Splenomegaly is an infrequent finding in reports of bacterial sepsis of the newborn. Palpate for bladder distension in the midline, above the symphysis pubis and below the umbilicus. Lymph nodes may be palpable in the neck, axilla, and/or groin in infants. Lymphoadenopathy has not been identified as a reliable indicator of neonatal sepsis.[10]
Palpate the femoral pulses. Compare femoral pulses to brachial pulses; both should be equal in intensity and timing. Diminished femoral pulses may indicate congenital heart disease, another consideration in the differential diagnosis of sepsis. Assess the capillary refill time (CFT) by applying pressure on the skin of the lower extremity until the skin blanches and monitor the time required for return of skin color. Flash CFT is seen in warm shock states and slow CFT (>2 seconds) indicates poor perfusion, a common finding associated with, but not specific to, sepsis.[16] Sclerema may also be present in sepsis (Fig 8).
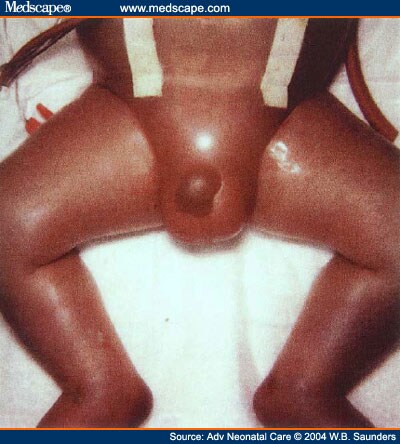
Figure 8. Note the swollen subcutaneous tissue and shiny edematous skin, often called sclerema; this is a late sign often associated with positive fluid balance in sepsis. Reprinted with permission from Clark D. Atlas of Neonatology. Philadelphia, Pa: WB Saunders; 2000:65.
Note the temperature of the skin. Normally the skin feels warm and dry. Poor perfusion results in skin that is cool to touch. The examiner should note the line of demarcation (i.e., skin cool to touch to the calf, to the thigh, groin, etc.). To identify potential sites of infection, inspect all existing and recent catheter insertion sites for redness, swelling, drainage, or pain. Palpate along the route of the indwelling catheter for edema. Palpate joints for edema, erythema, and decreased mobility as noted with osteomyelitis (Fig 9).

Figure 9. Systematic evaluation of the infant's joints may reveal a swollen joint associated with osteomyelitis. Photograph courtesy of Dr. David Clark, Albany Medical Center, Albany, New York.
Differential Diagnostic Considerations
In newborns, many conditions have a clinical presentation similar to sepsis and must be included in the differential diagnosis ( Table 5 ). These disorders need to be ruled out based on history, risk factors, and laboratory and radiologic findings.
Table 5.
| Condition | Similar to Sepsis |
|---|---|
| Neonatal drug withdrawal syndrome | Seizure activity |
| Irritability or persistent crying | |
| Alterations in temperature | |
| Gastrointestinal dysfunction | |
| Gastrointestinal dysfunction | |
| Respiratory conditions | |
| Respiratory distress syndrome | Tachypnea |
| Meconium aspiration syndrome | Retractions |
| Persistent pulmonary hypertension | Grunting |
| Air leaks | Nasal flaring |
| TTNB | Apnea |
| Pneumonia | Cyanosis |
| Exacerbation of BPD | Abnormal breath sounds |
Congenital abnormalities
|
|
| Gastrointestinal conditions | |
| Feeding intolerance | Abdominal distension |
| Gastrointestinal obstruction | Bowel loops |
| Necrotizing enterocolitis | Vomiting |
| Gastroesophageal reflux | Diarrhea |
| Gastric residuals | |
| Abdominal tenderness | |
| Erythematous areas | |
| Abnormal bowel sounds | |
| Organomegaly | |
| Congenital heart disease | Poor perfusion |
| Hypotension | |
| Tachycardia | |
| Bradycardia | |
| Arrhythmia | |
| Murmur | |
| Physiologic jaundice | Jaundice |
| Adrenal insufficiency [16] | Hypotension (persistent and refractory) |
| Congenital hypothyroidism [16] | Prolonged jaundice |
| Poor suck | |
| Poor feeding | |
| Lethargy | |
| Respiratory difficulties | |
| Bradycardia | |
| Intermittent cyanosis | |
| Dehydration | Poor perfusion |
| Tachycardia | |
| Hypotension | |
| Vaccine reaction | Alteration in temperature |
Abbreviations: TTNB, transient tachypnea of the newborn; BPD, bronchopulmonary dysplasia.
Table 5. Conditions With Similar Clinical Presentation to Infection and/or Sepsis[9,10,16]
To assist in the differential diagnosis of sepsis, several diagnostic tests are commonly utilized ( Table 6 ). Evaluate the results of these tests to complete your assessment of the infant. Newer diagnostic tests are currently being evaluated to improve the sensitivity and specificity of the diagnosis of sepsis and include procalcitonin and inflammatory mediators.[25,26]
Table 6.
| Name of Test | Outcomes | Indications |
|---|---|---|
Cultures
|
Presence of pathogens | Definitive isolation of microbial etiology |
| Gram stain | Presence of bacteria or yeast | Useful in directing antimicrobial therapy |
| Chest radiograph | Pulmonary infiltrates, edema | Pneumonia |
| Arterial blood gas | Low PCO2, low arterial pH, low bicarbonate | Complication of sepsis initially yielding respiratory alkalosis and later metabolic acidosis. |
| Neutrophils | Levels as low as 20% with rebound to 80% | Infection and sepsis progression |
| WBC | Elevated or elevated immature forms (left shift). | Infection |
| Total WBC <4000/mm3 | ||
| Immature to total ratio | ≥0.2 | Sepsis |
| C Reactive Protein [24] | In term or near-term infants, 2 serial measurements (12-24 hrs after onset of symptoms) >10 mg/L | Sepsis |
| Platelets | <100,000/microliter | Complications of sepsis (coagulation abnormality) |
| Glucose | Hypoglycemia | Sepsis |
| Hyperglycemia |
Abbreviation: PCO2; partial pressure of carbon dioxide; WBC, white blood cells.
Table 6. Tests Commonly Utilized in the Diagnosis of Sepsis[20-24]
Conclusion
Despite treatment, morbidity and mortality related to neonatal sepsis remain high. Tests currently used to diagnosis infection are neither sensitive nor specific in the neonatal period. A high index of suspicion, by the bedside provider, is the key to early recognition. International consensus definitions to define the continuum of sepsis and provide diagnostic criteria need to be further explored in the neonatal population. These definitions and diagnostic criteria do provide guidelines for the caregiver in evaluating whether the infant is exhibiting symptoms of a systemic inflammatory response. The bedside caregiver's ability to perform focused serial physical assessments for suspected sepsis, viewed in context of the history and available diagnostic data, remains a critical tool for the early identification and expedient treatment of sepsis in infants.
CE Information
The print version of this article was originally certified for CE credit. For accreditation details, contact the publisher, Elsevier, Inc., The Curtis Center, Independence Square West, Philadelphia, PA 19106.
References
- Hazelzet JA, DeGroot R. Sepsis-related problems in pediatric patients. In Sepsis: Current Perspectives in Pathology and Therapy, eds Reinhart K, Eyrich K, Sprung C. Berlin, Germany: Springer-Verlag; 1994. 217-227.
- Watson RS, Carcillo JA, Linde-Zwirble WT, Clermont G, Lidicker J. The epidemiology of severe sepsis in children in the United States. Am J Respir Care Med. 2003;167:695-701.
- Stoll BJ, Hansen N, Fararoff AA, Wright L, Carlo WA. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics 2002;110:285-291.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D. 2001 SCCM/ESICM/ACCP/ATS/SIS International sepsis definitions conference. Crit Care Med. 2003;31:1250-1256.
- American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864-874.
- Hayden WR. Sepsis terminology in pediatrics. J Pediatr. 1994;124:657-658.
- Manual of operations for infants born in 2004, 2004. Vermont Oxford Network [database online], Updated November 2003. Available at: http://www.vtoxford.org/2004Manual.pdf. Accessed January 5.
- NICHD Neonatal Research Network. Survey of morbidity and mortality among very low birth weight infants (401 to 1500 grams). Manual of Operations, 1998. Revised August 4.
- Donn Steven M. Neonatal infection. In The Michigan Manual: A Guide to Neonatal Intensive Care, eds Armonk, NY: Futura Publishing Company; 1997. 149-151.
- Klein JO. Bacterial sepsis and meningitis. In Infectious Disease of the Fetus and Newborn Infant, eds Remington JS, Klein JO. Philadelphia, Pa: WB Saunders Company; 2001. 964-975.
- Wolach B. Neonatal sepsis: pathogenesis and supportive therapy. Semin Perinatol 1997;21:28-38.
- Fowler EB, Breault LG, Cuenin MF. Periodontal disease and its association with systemic disease. Mil Med 2001;166:85-89.
- Joffe GM, Wright M. Prenatal environment: effect on neonatal outcome. In Handbook of Neonatal Intensive Care, eds Merenstein GB, Gardner SL. St. Louis, Mo: Mosby; 2002. 9-25.
- Ng PC, Cheng SH, Chui KM, Fok TF, Wong MY. Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birth weight infants. Arch Dis Child Fetal Neonatal Ed. 1997;77:221F-227F.
- Gardner SL, Goldson E. The neonate and the environment: impact on development. In Handbook of Neonatal Intensive Care, eds Merenstein GB, Gardner SL. St. Louis, Mo: Mosby; 2002. 225.
- Carcillo JA, Fields AI. Task Force Committee Members. Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med. 2002;30:1365-1378.
- Ruiz-Contreras J, Uriquia L, Bastero R. Persistent crying as predominant manifestation of sepsis in infants and newborns. Pediatr Emerg Care 1999;15:113-115.
- Martinot A, Leclerc F, Cremer R, Leteurtre S, Fourier C. Sepsis in neonates and children: definitions, epidemiology, and outcome. Pediatr Emerg Care 1997;13:277-281.
- Carvalho AC, Freeman NJ. How coagulation defects alter outcome in sepsis. J Crit Illn. 1994;9:51-75.
- Hardin TC, DiPiro JT. Sepsis and septic shock. In Pharmacotherapy, eds Stamford, Conn: Appleton and Lange; 1999. 1827-1838.
- Hoeprich PD, Jordan MC, Allan R. Sepsis and septic shock. In Infectious Diseases: A Treatise of Infectious Process, eds Hoeprich PD, Jordan MC, Ronald AR. Philadelphia, Pa: JB Lippincott; 1994. 511-515.
- Weinber GA, Powell KR. Laboratory aids for diagnosis of neonatal sepsis. In Infectious Disease of the Fetus and Newborn Infant, eds Remington JS, Klein JO. Philadelphia, Pa: WB Saunders Company; 2001. 1327-1340.
- Beers MH, Berkow R. Bacteremia and septic shock. In The Merck Manual, eds Whitehouse Station, NJ: Merck Research Labs; 2000. 1143-1147.
- Benitz W, Han M, Madan A, Ramachandra P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics 1998;102:e41. [serial online]. October, Available at: http://www.pediatrics.org/cgi/content/full/102/4/e41. Accessed September 19, 2003.
- Vincent JL. Procalcitonin: the marker of sepsis. Crit Care Med. 2000;28:1226-1227.
- Carlet J. Rapid diagnostic methods in the detection of sepsis. Infect Dis Clin North Am. 1999;13:483-491.
Authors and Disclosures
Mary A. Short, RN, MSN, Acute Care Division, Eli Lilly and Company, Lilly Corporate Center, Indianapolis, Ind
Disclosure: Mary A. Short, RN, MSN, is an employee and stockholder in Eli Lilly Company.
The author would like to thank Anne Schwoebel, RN, MSN, NNP, and Val Castrodale, RNC, MSN, NNP, for their review of this manuscript.
Funding InformationThis manuscript was solely supported by Eli Lilly and Company.
Reprint AddressMary A. Short, RN, MSN, Senior Therapeutic Associate, U.S. Affiliate, Acute Care Division, Eli Lilly and Company, Lilly Corporate Center, Indianapolis, IN 46285, Drop Code 6835 USA; Email: mshort@lilly.com
Adv Neonatal Care. 2004;4(3) © 2004 W.B. Saunders